This serious eye condition, if left untreated, can lead to permanent vision loss. Recognizing the early warning signs is crucial for timely intervention and preserving sight. The most common indicators include the sudden appearance of floaters, flashes of light, and a shadow or curtain obscuring part of your vision. Understanding these symptoms can empower you to seek prompt medical care.
What is Retinal Detachment?
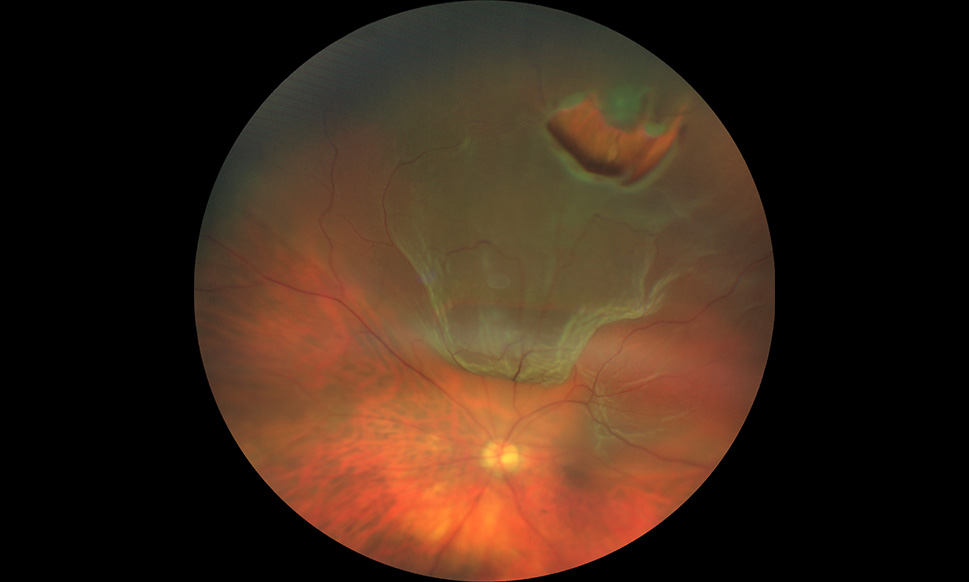
The retina is a thin layer of tissue at the back of the eye that receives light and sends images to your brain. When this layer detaches, it pulls away from the underlying tissue that supplies it with oxygen and nourishment. This separation is known as retinal detachment. There are different types of retinal detachment, but the most common is rhegmatogenous retinal detachment, which occurs when a tear or hole develops in the retina, allowing fluid to seep underneath and lift it away from the choroid.
Types of Retinal Detachment
- Rhegmatogenous Retinal Detachment: This is the most frequent type, caused by a tear or hole in the retina. It’s often associated with age-related changes in the vitreous gel.
- Tractional Retinal Detachment: This occurs when scar tissue on the retinal surface contracts and pulls the retina away from its normal position. It’s often seen in people with diabetes or other conditions that cause abnormal blood vessel growth.
- Exudative Retinal Detachment: In this type, fluid accumulates beneath the retina without a tear or hole. This can be caused by inflammatory conditions, tumors, or vascular diseases.
Key Warning Signs of Retinal Detachment
The most alarming symptoms of retinal detachment are often sudden and painless. They can appear individually or in combination.
1. Floaters
Floaters are small specks, dots, lines, or cobweb-like shapes that drift across your field of vision. While most people experience occasional floaters, a sudden increase in their number or size, especially when accompanied by other symptoms, is a significant warning sign. These “floaters” are actually small clumps of cells or protein within the vitreous humor, the gel-like substance that fills your eyeball. As the vitreous gel ages, it can liquefy and pull away from the retina, causing these clumps to become visible. In some cases, the pulling action on the retina can lead to a tear, initiating the detachment process.
- What to look for: New floaters that appear suddenly, particularly if they are numerous, dark, or resemble tiny insects or strings.
- When to worry: If you notice a significant increase in floaters, especially in conjunction with flashes of light or a loss of peripheral vision.
2. Flashes of Light (Photopsia)
Flashes of light, often described as seeing lightning streaks or camera flashes, can occur in one or both eyes. These flashes are typically seen in the peripheral vision and can appear intermittently. Like floaters, flashes of light are often caused by the vitreous gel pulling on the retina. This pulling stimulates the photoreceptor cells in the retina, which the brain interprets as light. These flashes can be brief or last for several seconds. They are not usually painful but can be quite startling.
- What to look for: Sudden, brief flashes of light, often seen in the side (peripheral) vision, that are not related to an external light source.
- When to worry: When flashes of light appear suddenly and persist, or are accompanied by an increase in floaters or a visual field defect.
3. A Shadow or Curtain in Your Vision
This is often the most concerning symptom, as it indicates that a significant portion of the retina may have detached. A shadow or curtain may appear to be descending over your vision, starting from the periphery and moving inwards. It can affect your central or peripheral vision, making it difficult to see clearly. This symptom suggests that the detached retina is no longer receiving oxygen and nutrients properly, impacting its function. The “curtain” sensation is due to the blind spot created by the detached retina.
- What to look for: A dark shadow or a gray curtain that seems to be covering a portion of your visual field.
- When to worry: If you notice any loss of vision, especially a progressive shadow or curtain, this is a medical emergency.
Other Potential Symptoms
While floaters, flashes, and shadows are the primary warning signs, other symptoms can sometimes accompany retinal detachment:
- Sudden decrease in vision: This can range from blurred vision to complete vision loss.
- Pain: While retinal detachment is often painless, some individuals may experience mild discomfort or a feeling of pressure in the eye.
- Distorted vision: Straight lines may appear wavy or bent, a phenomenon known as metamorphopsia.
Risk Factors for Retinal Detachment
Certain factors can increase an individual’s risk of developing retinal detachment:
Age
The risk of retinal detachment increases with age, particularly after the age of 50, due to natural changes in the vitreous gel.
Myopia (Nearsightedness)
Individuals with high myopia (severe nearsightedness) have a significantly higher risk. The elongated eyeball in myopia can lead to a thinner, more stretched retina, making it more prone to tears.
Previous Eye Surgery
Surgeries like cataract surgery or procedures to treat glaucoma can, in rare cases, increase the risk of retinal detachment.
Eye Injury
Trauma to the eye, whether blunt force or a penetrating injury, can cause tears in the retina that lead to detachment.
Family History
Having a family history of retinal detachment can increase your own risk.
Certain Eye Conditions
Conditions such as diabetic retinopathy, uveitis (inflammation inside the eye), and retinoschisis (a condition where the retina splits into layers) can predispose individuals to retinal detachment.
Also read: The Diabetic Eye: How Hyperglycemia Causes Microvascular Damage to the Retina
What to Do If You Experience Warning Signs
If you experience any of the warning signs of retinal detachment – a sudden increase in floaters, flashes of light, or a shadow in your vision – it is crucial to seek immediate medical attention. Do not wait to see if the symptoms improve. Retinal detachment is a medical emergency that requires prompt diagnosis and treatment to prevent permanent vision loss.
- Contact your ophthalmologist immediately: Your eye doctor can perform a comprehensive eye examination to determine if retinal detachment is present.
- Go to the nearest emergency room: If you cannot reach your eye doctor promptly, go to the nearest hospital emergency room, especially if you experience sudden vision loss.
- Avoid rubbing or pressing on your eye: This could potentially worsen the detachment.
Diagnosis and Treatment
An ophthalmologist can diagnose retinal detachment through a dilated eye examination. During this exam, they will use special instruments to view the retina and look for tears or detachment. Imaging tests, such as an ultrasound or optical coherence tomography (OCT), may also be used.
The treatment for retinal detachment depends on the type and severity of the detachment. Common treatment options include:
1. Pneumatic Retinopexy
This is a minimally invasive procedure where a gas bubble is injected into the eye to help push the detached retina back into place. The patient is then instructed to maintain specific head positions to allow the retina to reattach.
2. Scleral Buckle
In this surgical procedure, a silicone band (buckle) is placed around the outside of the eyeball. The buckle compresses the sclera (white part of the eye), pushing the eye wall inward against the detached retina, helping it to reattach.
3. Vitrectomy
This is a more extensive surgery where the vitreous humor is removed from the eye. The surgeon then uses instruments to flatten the retina and may inject a gas bubble or silicone oil to keep the retina in place while it heals.
4. Laser Photocoagulation or Cryopexy
These techniques are often used to treat retinal tears before they lead to detachment. Laser photocoagulation uses a laser to create tiny burns around the tear, forming scar tissue that seals it. Cryopexy uses extreme cold to freeze the area around the tear, also creating scar tissue to seal it.
The Importance of Regular Eye Exams
Regular comprehensive eye exams are vital for maintaining eye health and detecting potential problems early. For individuals with risk factors for retinal detachment, such as high myopia or a family history, more frequent check-ups may be recommended by their eye care professional. Early detection is key to successful treatment and preserving vision.
Retinal detachment is a serious condition that can lead to irreversible vision loss if not treated promptly. The hallmark warning signs – sudden floaters, flashes of light, and a shadow or curtain in your vision – should never be ignored. If you experience any of these symptoms, seek immediate medical attention from an ophthalmologist. Understanding the risks and symptoms can empower you to protect your precious sight. Early intervention significantly improves the chances of a successful outcome and the preservation of your vision.
Frequently Asked Questions (FAQ)
Q1: Are floaters always a sign of retinal detachment?
No, floaters are very common and often caused by normal aging of the vitreous gel. However, a sudden increase in floaters, especially with other symptoms, warrants immediate medical attention.
Q2: Can retinal detachment be painless?
Yes, retinal detachment is often painless. The primary symptoms are visual disturbances like floaters, flashes, and vision loss, not pain.
Q3: How quickly does vision loss occur with retinal detachment?
Vision loss can occur rapidly once a significant portion of the retina detaches. Prompt treatment is essential to minimize permanent vision damage.
Q4: Can I still see if I have a retinal detachment?
It depends on the extent of the detachment. You might still have some vision, particularly if the detachment is peripheral. However, a shadow or curtain in your vision indicates a loss of visual field.
Q5: What is the success rate of retinal detachment surgery?
Success rates for retinal reattachment surgery are generally high, often exceeding 80-90%, especially with prompt treatment. However, full vision recovery can vary and may depend on factors like the duration of detachment and the presence of other eye conditions.
Q6: Is there anything I can do to prevent retinal detachment?
While not all cases can be prevented, managing underlying conditions like diabetes, protecting your eyes from injury, and seeking regular eye exams, especially if you have risk factors, can help reduce your risk.