Did you know that approximately 50% of patients undergoing cataract surgery experience some degree of dry eye disease? This common condition, often overlooked, can significantly impact the success of your vision correction procedure and your overall visual recovery. At Fathima Eye Care Hospital, we understand the intricate connection between dry eye and cataract surgery, and we emphasize proactive management for the best possible outcomes.
Understanding Dry Eye Disease
Dry eye disease, also known as dry eye syndrome, is a chronic condition characterized by the eyes’ inability to produce enough tears or the tears evaporating too quickly. This leads to discomfort, including stinging, burning, redness, and a gritty sensation. Tears are vital for lubricating the eye’s surface, washing away debris, and maintaining clear vision. When this delicate balance is disrupted, various symptoms can arise.
Causes of Dry Eye
Several factors can contribute to dry eye:
· Age: Tear production naturally decreases with age, making older adults more susceptible.
· Gender: Women are more prone to dry eye, especially after menopause.
· Medical Conditions: Conditions like Sjogren’s syndrome, rheumatoid arthritis, and lupus can affect tear production.
· Medications: Certain medications, including antihistamines, decongestants, antidepressants, and blood pressure medications, can reduce tear flow.
· Environmental Factors: Exposure to wind, smoke, dry air, and prolonged screen time can exacerbate dry eye.
· Eyelid Problems: Conditions like blepharitis (inflammation of the eyelids) can disrupt the oil glands that keep tears from evaporating too quickly.
Symptoms of Dry Eye
Common symptoms include:
- A stinging, burning, or scratchy sensation in the eyes.
- Redness.
- A feeling of having something in the eye.
- Blurred vision that improves with blinking.
- Sensitivity to light.
- Eye fatigue.
- Watery eyes (a paradoxical symptom as the eye tries to compensate for dryness).
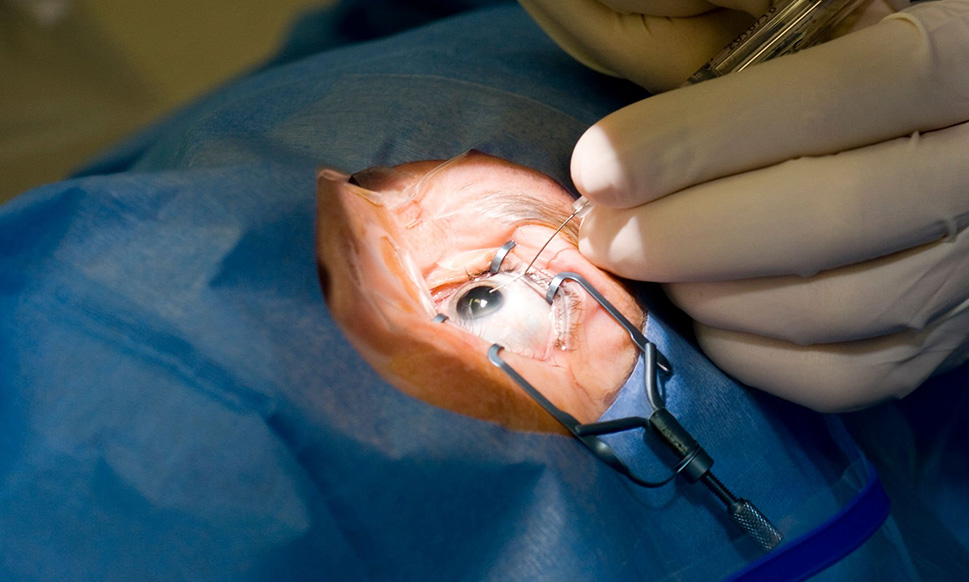
The Critical Link: Dry Eye and Cataract Surgery
Cataract surgery involves removing the clouded natural lens and replacing it with an artificial intraocular lens (IOL). While a highly successful procedure, it can temporarily worsen pre-existing dry eye or even trigger new symptoms. Understanding why this happens is crucial for effective management.
How Cataract Surgery Can Affect Dry Eye
Inflammation: The surgical process itself causes a degree of inflammation on the eye’s surface. This inflammation can disrupt the tear film and worsen dryness.
Nerve Disruption: The cornea, the clear front part of the eye, is rich in nerves that help regulate tear production and sensation. Microscopic incisions made during surgery can temporarily affect these nerves, reducing the eye’s ability to signal for lubrication.
Changes in Tear Film Stability: The surgical environment and the introduction of new surfaces (the IOL) can alter the normal stability of the tear film, leading to faster evaporation.
Medications: Post-operative eye drops, while essential for healing, can sometimes have a drying effect.
Why Pre-Operative Dry Eye Management is Essential
Ignoring or neglecting dry eye before cataract surgery can lead to several complications and suboptimal results. Proactive management, often starting weeks or months before your procedure at Fathima Eye Care Hospital, is key.
1. Improved Visual Acuity and IOL Calculations
- Accurate Measurements: The accuracy of the measurements taken to determine the power of your new intraocular lens (IOL) is paramount. Dry eyes can cause fluctuations in the corneal surface. An irregular or dry cornea can lead to inaccurate readings during the diagnostic tests (like biometry) used to calculate the correct IOL power. This can result in a less precise visual outcome after surgery, potentially leading to residual refractive errors (needing glasses for distance or near vision more than expected).
- Clearer Vision Post-Surgery: A stable tear film is essential for clear vision. If dry eye persists or worsens after surgery, it can significantly obscure the sharp vision that the new IOL is designed to provide. Even with a perfectly placed IOL, a dry, irregular cornea will prevent light from focusing properly.
2. Enhanced Comfort and Reduced Post-Operative Discomfort
- Minimizing Irritation: Post-operative recovery involves a period of healing and adaptation. If you are already suffering from dry eye symptoms, the added irritation from the surgical site can make this recovery period much more uncomfortable. Managing dry eyes beforehand can lead to a smoother, more pleasant healing process.
- Reducing Burning and Stinging: The stinging and burning associated with dry eye can be amplified after surgery, making it harder to keep your eyes comfortable and focused.
3. Better Healing and Reduced Risk of Infection
- Healthy Ocular Surface: A healthy, well-lubricated ocular surface is more conducive to proper healing. Dryness can impair the eye’s natural defense mechanisms, making it more vulnerable.
- Lower Infection Risk: While rare, infections are a serious risk after any surgery. A compromised ocular surface due to severe dry eye might theoretically increase this risk, although modern surgical techniques and antibiotic use significantly minimize this.
4. More Reliable Refractive Outcomes
- Predictable Vision: The goal of cataract surgery is not just to remove the cataract but often to improve your overall vision and reduce your dependence on glasses. If dry eye is not managed, the final visual outcome can be less predictable and may not meet your expectations. For patients seeking monovision (one eye corrected for distance, the other for near) or multifocal IOLs, the stability of the tear film is even more critical for achieving the intended visual benefits.
5. Patient Satisfaction and Quality of Life
- Achieving Goals: Ultimately, patients undergo cataract surgery to see better and improve their quality of life. Persistent dry eye symptoms after surgery can diminish the perceived benefits of the procedure, leading to dissatisfaction. Addressing dry eyes beforehand ensures patients can fully appreciate the improved vision and enjoy their daily activities without discomfort.
Also read: Amblyopia (Lazy Eye): Why Early Intervention is Critical for Neural Development
Strategies for Managing Dry Eye Before Cataract Surgery
At Fathima Eye Care Hospital, we employ a multi-faceted approach to manage dry eye effectively before your cataract surgery. The specific treatment plan will be tailored to your individual needs based on a thorough eye examination.
1. Artificial Tears and Lubricants
- Frequent Use: Over-the-counter artificial tears are often the first line of defense. They provide temporary relief by supplementing natural tears. Preservative-free options are generally recommended for frequent use to avoid potential irritation from preservatives.
- Gels and Ointments: For more severe dryness, thicker gels or ointments may be prescribed for use at bedtime to provide longer-lasting lubrication.
2. Prescription Eye Drops
- Anti-inflammatory Drops: In cases where inflammation is a significant factor, your eye doctor may prescribe corticosteroid or cyclosporine eye drops to reduce inflammation and increase tear production.
- Cholinergic Agonists: Medications like pilocarpine can sometimes be used to stimulate tear production.
3. Lifestyle and Environmental Modifications
- Blink More Often: When using digital devices, consciously remind yourself to blink fully and frequently. This helps spread tears across the eye’s surface.
- Take Screen Breaks: Follow the 20-20-20 rule: every 20 minutes, look at something 20 feet away for at least 20 seconds.
- Humidify Your Environment: Use a humidifier at home or work, especially during dry seasons or in air-conditioned environments.
- Avoid Irritants: Steer clear of smoke, strong winds, and direct air vents. Wear wraparound sunglasses outdoors to protect your eyes.
4. Eyelid Hygiene
- Warm Compresses: Applying warm compresses to the eyelids can help melt blockages in the meibomian glands, which produce the oily layer of the tear film. This is particularly helpful for meibomian gland dysfunction (MGD), a common cause of evaporative dry eye.
- Eyelid Scrubs: Gentle cleaning of the eyelids with specialized eyelid cleansers can remove debris and bacteria that contribute to inflammation like blepharitis.
5. Nutritional Supplements
- Omega-3 Fatty Acids: Studies suggest that omega-3 fatty acid supplements (found in fish oil and flaxseed oil) can help improve the quality of the tear film and reduce inflammation associated with dry eye.
6. Advanced Treatments
- Punctal Plugs: Tiny devices called punctal plugs can be inserted into the tear ducts to slow down the drainage of tears from the eye’s surface, keeping it more lubricated.
- Scleral Lenses: For severe dry eye, specialized scleral contact lenses can create a fluid-filled reservoir over the cornea, providing continuous lubrication and protection.
The Fathima Eye Care Hospital Approach
Our ophthalmologists at Fathima Eye Care Hospital conduct a comprehensive evaluation to diagnose the type and severity of your dry eye. This includes assessing tear production, tear film stability, and the health of your eyelids and meibomian glands.
Based on these findings, we will develop a personalized treatment plan aimed at optimizing your ocular surface health before your cataract surgery. This may involve a combination of the strategies listed above. We believe that addressing dry eye proactively is not just about managing a symptom; it’s about ensuring you achieve the best possible vision and comfort after your life-changing cataract surgery.
Conclusion
Dry eye disease is far more than just a minor annoyance; it’s a significant factor that can influence the success and recovery from cataract surgery. By understanding its impact and actively managing it before your procedure, you pave the way for clearer vision, greater comfort, and a more satisfying outcome. Don’t let dry eyes compromise your sight. Consult with the experts at Fathima Eye Care Hospital to discuss your dry eye concerns and ensure your journey to improved vision is as smooth and successful as possible.
Frequently Asked Questions (FAQ)
Q1: Will cataract surgery make my dry eye worse?
Cataract surgery can temporarily worsen pre-existing dry eye symptoms or even trigger new ones due to inflammation and changes in corneal nerves. Proactive management is key.
Q2: How long before cataract surgery should I start managing my dry eye?
Ideally, you should begin managing dry eye several weeks to months before surgery to optimize your ocular surface health.
Q3: Can dry eye affect the results of my cataract surgery?
Yes, significant dry eye can affect the accuracy of measurements for your intraocular lens (IOL) and lead to less predictable visual outcomes and reduced visual quality post-surgery.
Q4: What are the most common treatments for dry eye before cataract surgery?
Common treatments include artificial tears, prescription eye drops, lifestyle changes, eyelid hygiene, and sometimes punctal plugs.
Q5: Should I tell my eye doctor if I have dry eye symptoms?
Absolutely. It is crucial to inform your ophthalmologist about any dry eye symptoms you experience, as it directly impacts surgical planning and outcomes.
Q6: Are there any risks associated with treating dry eye before surgery?
Generally, treatments for dry eye are safe. Some prescription drops may have minor side effects, but the benefits of managing dry eye before surgery far outweigh potential risks. Discuss all concerns with your doctor.