Did you know that approximately one-third of adults with diabetes have some form of diabetic retinopathy, a leading cause of vision loss in working-age adults? This staggering statistic highlights the critical need to understand how high blood sugar levels, a hallmark of diabetes, can silently wreak havoc on the delicate tissues of the eye, particularly the retina.
Diabetes, a chronic condition characterized by persistently elevated blood glucose (sugar) levels, affects millions worldwide. While the systemic effects of diabetes are well-documented, its impact on the eyes is often underestimated until significant vision impairment occurs. The primary culprit behind this visual deterioration is a process known as microvascular damage to the retina, directly driven by hyperglycemia – the medical term for high blood sugar.
This article will delve into the intricate mechanisms by which hyperglycemia damages the retina’s tiny blood vessels, leading to diabetic eye disease. We will explore the stages of this condition, its symptoms, risk factors, and the crucial importance of regular eye examinations and proactive management to preserve vision. For those seeking expert care and advanced treatments for eye conditions, including diabetic eye disease, Fathima Eye Care Hospital offers comprehensive services.
Understanding the Retina and Its Microvasculature
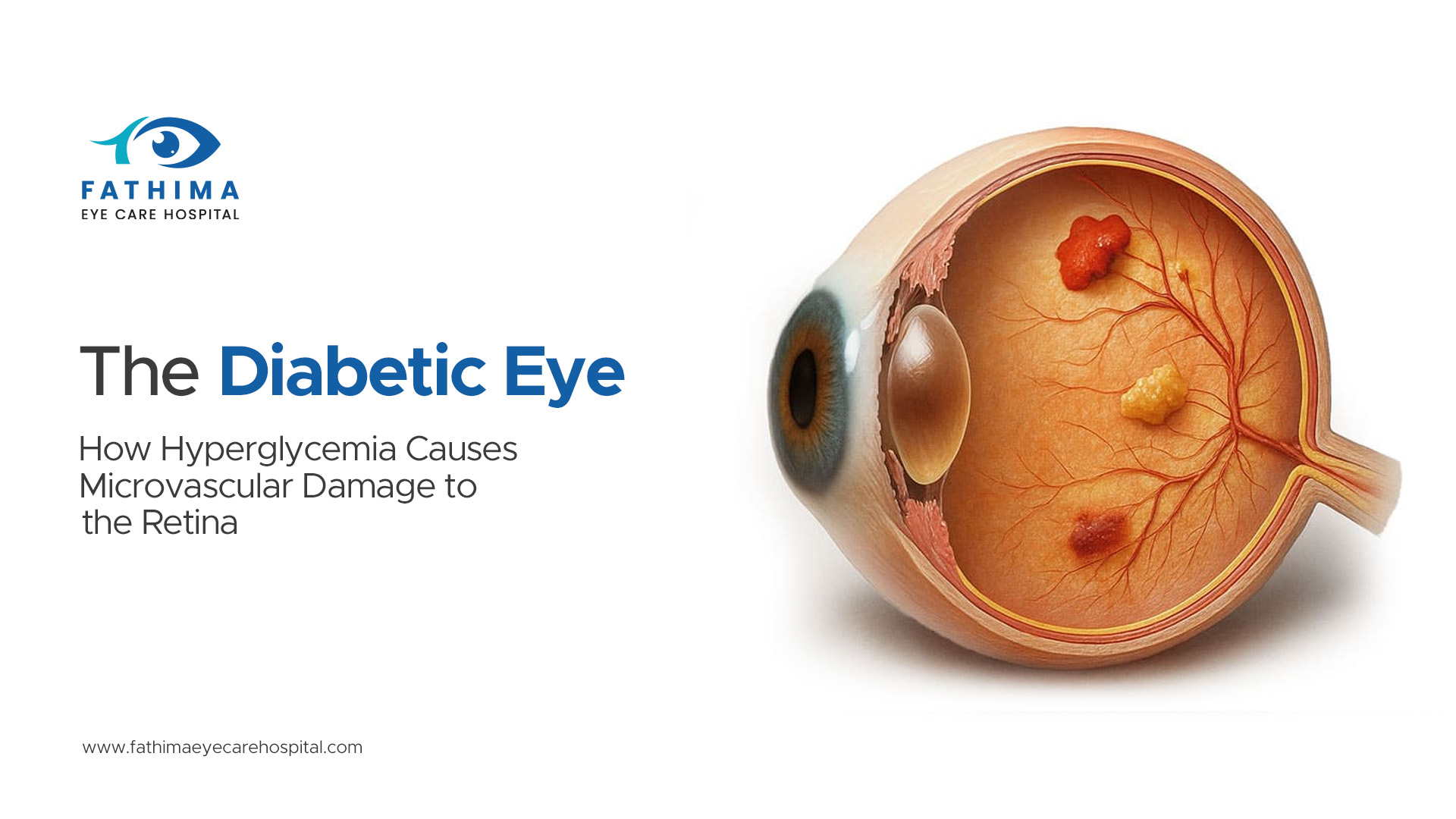
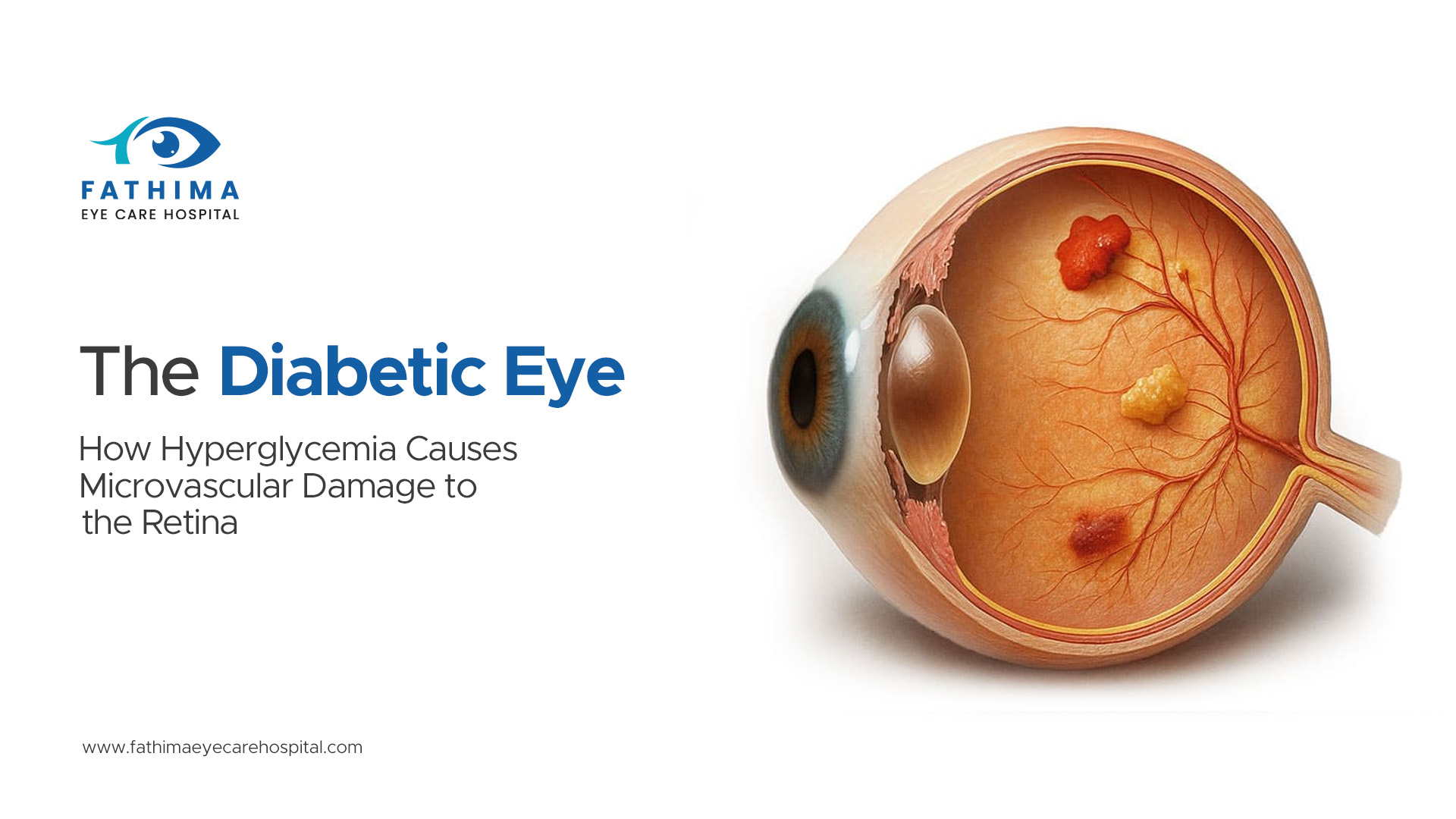
The retina is a light-sensitive layer of tissue at the back of the eye. It’s responsible for converting light into electrical signals that are then sent to the brain, allowing us to see. This intricate organ is densely packed with photoreceptor cells (rods and cones) and a complex network of blood vessels. These blood vessels, known as microvasculature, are incredibly small and supply the retina with the oxygen and nutrients it needs to function properly.
The health of these microvessels is paramount. They are so fine that even slight changes can have profound consequences. In individuals with diabetes, persistently high blood sugar levels can compromise the integrity and function of this vital network.
The Vicious Cycle: Hyperglycemia’s Impact on Retinal Blood Vessels
Hyperglycemia sets off a cascade of damaging biochemical reactions within the retinal microvasculature. The elevated glucose levels lead to several key pathological processes:
1. Advanced Glycation End Products (AGEs)
When glucose levels are high, glucose molecules can attach to proteins and lipids in a process called glycation. Over time, these glycated molecules undergo further chemical modifications to form Advanced Glycation End Products (AGEs). AGEs are harmful compounds that accumulate in blood vessel walls, making them stiffer, less flexible, and more prone to damage. They also contribute to inflammation and oxidative stress within the retinal vessels.
2. Oxidative Stress
Hyperglycemia significantly increases the production of reactive oxygen species (ROS), also known as free radicals. This imbalance between ROS production and the body’s ability to neutralize them is called oxidative stress. Oxidative stress damages cellular components, including the endothelial cells that line the blood vessels. This damage weakens the vessel walls, making them leaky and prone to abnormal growth.
3. Activation of the Polyol Pathway
In high glucose environments, an enzyme called aldose reductase becomes overactive. It diverts glucose away from its normal metabolic pathways into the polyol pathway. This pathway leads to the accumulation of sorbitol, a sugar alcohol, within cells. Sorbitol can disrupt cell function and contribute to oxidative stress and damage to the nerve cells in the retina.
4. Inflammation
Hyperglycemia triggers a chronic inflammatory response within the retinal blood vessels. Inflammatory markers are elevated, leading to further damage to the vessel walls and promoting the leakage of fluid and blood into the retinal tissue.
Stages of Diabetic Eye Disease
Diabetic eye disease, primarily diabetic retinopathy, typically progresses through several stages:
Non-Proliferative Diabetic Retinopathy (NPDR)
This is the earliest stage. In NPDR, the small blood vessels in the retina begin to weaken and leak. This leakage can cause:
- Microaneurysms: Tiny bulges or balloon-like sacs that form on the walls of the blood vessels. These are often the first visible signs of diabetic retinopathy.
- Hemorrhages: Small bleeds from the weakened vessels.
- Exudates: Leaky vessels can release fluid and lipids, which appear as yellowish deposits on the retina.
At this stage, vision may not be significantly affected, or there might be mild blurring. However, the underlying damage is progressing.
Proliferative Diabetic Retinopathy (PDR)
This is a more advanced and serious stage. As the damage to the existing blood vessels worsens, the retina tries to compensate by growing new, abnormal blood vessels. This process is called neovascularization.
These new blood vessels are fragile and abnormal. They:
- Bleed easily: Leading to significant hemorrhages within the eye, which can cause sudden and severe vision loss.
- Can cause scar tissue: The abnormal vessels can lead to the formation of scar tissue, which can pull on the retina.
- Lead to retinal detachment: If the scar tissue pulls too hard, it can detach the retina from its underlying support, a condition called tractional retinal detachment. This is a medical emergency and can lead to permanent blindness if not treated promptly.
- Cause neovascular glaucoma: The abnormal blood vessels can also grow in the front part of the eye, blocking the drainage of fluid and leading to a dangerous increase in eye pressure, known as neovascular glaucoma. This can severely damage the optic nerve and lead to irreversible vision loss.
Diabetic Macular Edema (DME)
Diabetic Macular Edema (DME) is a common complication of both NPDR and PDR. The macula is the central part of the retina responsible for sharp, detailed vision (reading, recognizing faces). In DME, fluid leaks from damaged blood vessels into the macula, causing it to swell.
This swelling distorts vision, making straight lines appear wavy and causing blurry or reduced central vision. DME is a major cause of vision loss in people with diabetes.
Symptoms of Diabetic Eye Disease
In the early stages, diabetic retinopathy often has no symptoms. This is why regular eye exams are so critical. As the condition progresses, symptoms may include:
- Blurred or fluctuating vision: Blood sugar levels that change can cause temporary vision changes. Swelling in the macula can also cause blurriness.
- Floaters: Small specks or dark strings that appear to float in your field of vision. These are often caused by bleeding into the eye.
- Sudden vision loss: This can occur due to significant bleeding or retinal detachment.
- Dark or empty areas in your vision: Indicating areas of vision loss.
- Difficulty seeing at night.

Also read: A Day-by-Day Guide to Biological Healing After Eye Surgery
Risk Factors for Diabetic Eye Disease
While diabetes is the primary risk factor, several other factors can increase the likelihood and severity of diabetic eye disease:
- Duration of diabetes: The longer a person has diabetes, the higher their risk.
- Poor blood sugar control: Consistently high A1C levels are strongly associated with an increased risk of diabetic eye complications. According to the American Diabetes Association, maintaining an A1C goal of below 7% can significantly reduce the risk of microvascular complications.
- High blood pressure (Hypertension): Uncontrolled high blood pressure can further damage blood vessels throughout the body, including those in the eyes.
- High cholesterol: Elevated cholesterol levels can contribute to the hardening and narrowing of blood vessels.
- Kidney disease (Nephropathy): Diabetic kidney disease often goes hand-in-hand with diabetic eye disease, as both are microvascular complications.
- Pregnancy: Hormonal changes during pregnancy can sometimes worsen diabetic retinopathy.
- Smoking: Smoking damages blood vessels and can exacerbate diabetic eye disease.
Diagnosis and Monitoring
Early detection and regular monitoring are key to managing diabetic eye disease. An eye care professional will perform a comprehensive dilated eye exam, which typically includes:
- Visual Acuity Test: To check how well you can see at different distances.
- Dilated Fundus Examination: Eye drops are used to widen the pupils, allowing the doctor to get a clear view of the retina, optic nerve, and blood vessels. The doctor looks for signs of microaneurysms, hemorrhages, exudates, and abnormal blood vessel growth.
- Optical Coherence Tomography (OCT): This non-invasive imaging test uses light waves to create cross-sectional images of the retina, helping to detect swelling (edema) and other structural changes.
- Fluorescein Angiography: In this test, a special dye is injected into a vein in your arm. As the dye circulates through the blood vessels in your eyes, a camera takes rapid photographs of the retina, highlighting areas of leakage or blockage.
Treatment and Management
The primary goal of treatment is to slow or stop the progression of diabetic eye disease and preserve vision. Management strategies include:
1. Blood Sugar Control
This is the cornerstone of preventing and managing diabetic eye disease. Maintaining optimal blood glucose levels through diet, exercise, and medication (as prescribed by your doctor) is crucial. The landmark Diabetes Control and Complications Trial (DCCT) and its follow-up, the Epidemiology of Diabetes Interventions and Complications (EDIC) study, demonstrated a significant reduction in the risk of diabetic retinopathy progression with intensive blood glucose control.
2. Blood Pressure and Cholesterol Management
Controlling hypertension and hyperlipidemia is also vital, as these conditions can worsen retinal damage.
3. Medications
- Anti-VEGF Injections: Vascular Endothelial Growth Factor (VEGF) is a protein that promotes the growth of abnormal blood vessels. Medications like ranibizumab (Lucentis), aflibercept (Eylea), and bevacizumab (Avastin) are injected directly into the eye to block VEGF, reduce leakage, and slow the growth of abnormal vessels. These are highly effective for treating DME and PDR.
- Corticosteroids: Steroid medications, in the form of injections or eye drops, can also be used to reduce inflammation and swelling in the macula.
4. Laser Treatment (Photocoagulation)
- Focal Laser Treatment: Used to seal leaking microaneurysms in specific areas of the retina, particularly for DME.
- Scatter Laser Treatment (Panretinal Photocoagulation): Used in PDR to shrink abnormal blood vessels by creating small burns in the peripheral retina. This reduces the retina’s demand for oxygen and can prevent further growth of abnormal vessels and reduce bleeding.
5. Surgery
- Vitrectomy: This surgical procedure is performed when significant bleeding or scar tissue is present, or if there is retinal detachment. The surgeon removes the vitreous gel (the jelly-like substance filling the eye) and any scar tissue, and may repair retinal detachments.
Prevention is Key
While diabetes can be a challenging condition, proactive management can significantly reduce the risk and impact of diabetic eye disease. Here’s how:
- Regular Dilated Eye Exams: Schedule an eye exam at least annually, or more often if recommended by your eye doctor, especially if you have diabetes. Early detection is crucial.
- Achieve and Maintain Good Blood Sugar Control: Work closely with your healthcare team to keep your blood glucose levels within the target range.
- Manage Blood Pressure and Cholesterol: Follow your doctor’s advice for managing hypertension and high cholesterol.
- Healthy Lifestyle: Adopt a balanced diet, engage in regular physical activity, and avoid smoking.
- Understand Your Risk: Be aware of the risk factors and discuss them with your doctor.
Hyperglycemia is a silent, yet potent, destroyer of the delicate microvasculature of the retina. The persistent elevation of blood sugar levels initiates a cascade of damaging processes that can lead to diabetic retinopathy, diabetic macular edema, and ultimately, irreversible vision loss. However, by understanding the mechanisms of damage, recognizing the symptoms, and committing to proactive management – including regular eye exams, diligent blood sugar control, and a healthy lifestyle – individuals with diabetes can significantly reduce their risk and protect their precious sight. Early intervention and ongoing care, such as that provided by Fathima Eye Care Hospital, are paramount in preserving vision and maintaining quality of life for those affected by diabetes.
Frequently Asked Questions (FAQs)
Q1: Can diabetic eye disease be completely cured?
While diabetic eye disease cannot always be completely cured, especially if it has progressed significantly, it can often be effectively managed and its progression slowed or stopped with timely treatment and diligent management of diabetes. Early detection and intervention are key to preserving vision.
Q2: How often should someone with diabetes have an eye exam?
People with diabetes should have a comprehensive dilated eye exam at least once a year. If you have existing diabetic retinopathy or other risk factors, your eye doctor may recommend more frequent check-ups.
Q3: Does everyone with diabetes develop eye problems?
No, not everyone with diabetes develops severe eye problems. However, the risk is significantly elevated compared to the general population. Good blood sugar control and regular eye exams can greatly reduce the chances of developing serious complications.
Q4: Can I still have good vision if I have diabetic retinopathy?
In the early stages (non-proliferative diabetic retinopathy), vision may be unaffected or only mildly blurred. With treatment and good diabetes management, many people can maintain good functional vision. However, advanced stages (proliferative diabetic retinopathy and severe macular edema) can lead to significant and sometimes irreversible vision loss.
Q5: What is the most important thing I can do to prevent diabetic eye disease?
The single most important thing is to maintain excellent control of your blood sugar levels. Additionally, regular dilated eye exams are crucial for early detection and intervention.
Q6: Are there any natural remedies for diabetic eye disease?
While a healthy diet and lifestyle are essential for managing diabetes and overall eye health, there are no scientifically proven natural remedies that can cure or effectively treat diabetic eye disease. Medical treatments, such as injections, laser therapy, and surgery, along with strict blood sugar control, are the established methods for managing the condition.