Diabetes has been a major lifestyle health hazard that has inversely affected the life of millions of people worldwide. Among those serious complications created by this life-style disease, Vision- loss is the least known or rather less discussed long term diabetes complication that needs an early intervention and prevention. Here, let’s try to explore how diabetes and vision are related, how this life-style disease hampers your vision, the specific conditions associated with it, and what individuals can do to ensure proper diabetes eye care.
Understanding Diabetes
Before exploring the connection between diabetes and vision loss, it’s important to understand what diabetes is. There are primarily two types:
- Type 1 Diabetes: An autoimmune condition where the body does not produce insulin.
- Type 2 Diabetes: More common, this type occurs when the body becomes resistant to insulin or doesn’t produce enough.
Regardless of the type, high blood sugar levels can lead to various complications, including those affecting the eyes.
How Diabetes Affects Vision
Diabetes and Vision, though less discussed, has always been a matter of medical anxiety where prolonged diabetic conditions can cause several eye problems, primarily due to long term high blood sugar levels that damage blood vessels in the body. This includes the tiny vessels in the eyes, leading to various eye diseases. Some of the most significant conditions linked to diabetes include:
1. Diabetic Retinopathy
Diabetic retinopathy is the most common cause of vision loss among people with diabetes. It occurs when high blood sugar levels damage the blood vessels in the retina, the light-sensitive tissue at the back of the eye. This can always be a permanent damage that can cause the vessels to leak fluid or bleed, leading to vision problems.
There are two main stages of diabetic retinopathy:
- Non-proliferative Diabetic Retinopathy (NPDR): This early stage involves the swelling and leaking of blood vessels. It may not cause noticeable symptoms initially.
- Proliferative Diabetic Retinopathy (PDR): This more advanced stage occurs when new, abnormal blood vessels begin to grow in the retina, which can lead to severe vision loss.
2. Diabetic Macular Edema
Diabetic macular edema (DME) is a complication of diabetic retinopathy. It occurs when fluid leaks into the macula, the central part of the retina responsible for sharp vision. DME can happen at any stage of diabetic retinopathy and can significantly impact central vision.
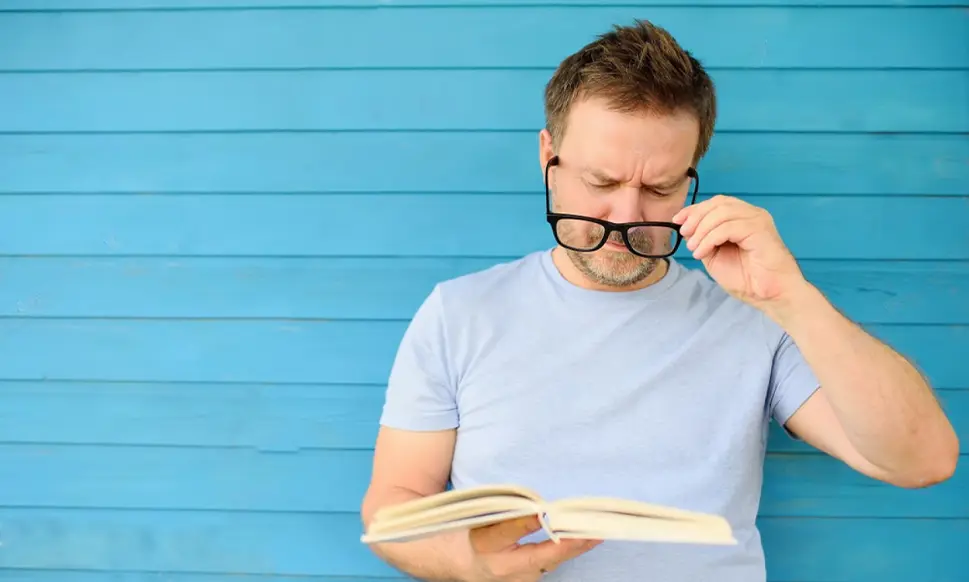
3. Cataracts
People with diabetes are more prone to developing early cataracts, a clouding of the lens of the eye that can lead to blurry vision. Cataracts tend to develop at an earlier age in people with diabetes, and they can progress more rapidly.
Also read : Cataract Care Made Simple: Discover Our Painless, Injection-Less Approach
4. Glaucoma
Diabetes increases the risk of glaucoma, a group of eye conditions that damage the optic nerve, often due to high eye pressure. Glaucoma can lead to vision loss if not treated promptly. People with diabetes are at higher risk of developing open-angle glaucoma and other types.
Also read : Understanding Glaucoma: What You Should Know About This Silent Vision Thief

Symptoms to Take Care
Recognizing the early signs of eye complications due to diabetes is vital. Common symptoms include:
- Blurred or fluctuating vision
- Dark or empty areas in vision
- Difficulty seeing at night
- Colors appearing faded or washed out
- Sudden vision loss
If you experience any of these symptoms, it’s essential to consult an eye care professional promptly.
Risk Factors
Several factors can increase the likelihood of developing vision complications due to diabetes, including:
- Duration of Diabetes: The longer a person has diabetes, the higher the risk of developing eye complications.
- Blood Sugar Control: Poorly managed blood sugar levels can accelerate the development of eye diseases.
- Hypertension: High blood pressure can exacerbate eye issues in people with diabetes.
- Cholesterol Levels: High cholesterol can contribute to the risk of diabetic eye disease.
- Smoking: Tobacco use can further damage blood vessels, increasing the risk of eye complications.
Prevention and Management
While the risk of vision loss from diabetes is significant, there are effective strategies to prevent and manage eye complications.
1. Regular Eye Exams
Diabetic eye tests are crucial for early detection of diabetic eye diseases. The American Diabetes Association recommends that individuals with diabetes have a comprehensive dilated diabetic eye Test at least once a year. This allows for early intervention and treatment.
2. Blood Sugar Management
Maintaining optimal blood sugar levels is vital in reducing the risk of developing diabetes-related eye diseases. This can involve:
- Monitoring blood glucose regularly
- Following a balanced diet rich in whole foods, fiber, and low in processed sugars
- Engaging in regular physical activity
- Adhering to prescribed medications
3. Manage Blood Pressure and Cholesterol
Keeping blood pressure and cholesterol levels within recommended ranges is important for overall health, including eye health. This may involve lifestyle changes, such as diet and exercise, and possibly medication.
4. Avoid Smoking
Quitting smoking can significantly reduce the risk of developing diabetic eye diseases and other complications related to diabetes.
5. Protect Your Eyes
Wearing sunglasses that block UV rays can protect your eyes from damage. Additionally, ensure that your living and work environments are well-lit to reduce strain on your eyes.
Also read : 7 Common Eye Problems in Children and How to Address Them
Treatment Options
If diabetic eye disease is diagnosed, several treatment options may be available:
- Laser Treatment: For diabetic retinopathy, laser treatment can help seal leaking blood vessels or reduce abnormal blood vessel growth.
- Injections: Medications can be injected into the eye to reduce swelling and inhibit the growth of abnormal blood vessels in cases of DME.
- Surgery: In severe cases, surgery may be necessary to address retinal detachment or other complications.
The link between diabetes and vision loss is significant and can lead to severe consequences if not addressed. Understanding the risks, recognizing the symptoms, and taking proactive measures can help protect your vision. Regular diabetic eye exams, effective blood sugar and eye health management, and lifestyle changes are essential components in safeguarding your eyesight. If you or a loved one has diabetes, prioritize eye health to ensure a better quality of life. By staying informed and vigilant, you can mitigate the risks associated with diabetes and maintain your vision for years to come.
At Fathima Eye Care, we are dedicated to helping you preserve your vision and health. If you’re concerned about diabetes-related eye issues or need a comprehensive eye exam, don’t wait. Contact us today to schedule your appointment and ensure your eyes receive the care they deserve. Together, we can take the necessary steps to protect your eyesight and improve your quality of life. Your vision matters, let us help you safeguard it!